In an effort to make the MIPS submission process less stressful for small practices, the Centers for Medicare and Medicaid Services (CMS) has altered the parameters of reporting for MIPS if your practice consists of 15 clinicians or less. The following guide will explain how to best prepare your MIPS data if you are a small practice.
What is the Same?
Many elements of the MIPS submission and reporting processes are the same whether you are small practice or not. Small practices will have the opportunity to select the reporting option that works best for them, including traditional MIPS, MIPS APM, and the newest reporting option MVPs. You will also have the same options in terms of your participation, and will be able to report as an individual, group, virtual group, APM entity, or subgroup depending on what’s best for you.
The Quality and Improvement Activities Performance Categories will remain mostly unchanged between large and small practices, as will the process of determining and verifying your eligibility. The process of submitting your data will also mostly remain unchanged.
What is Different?
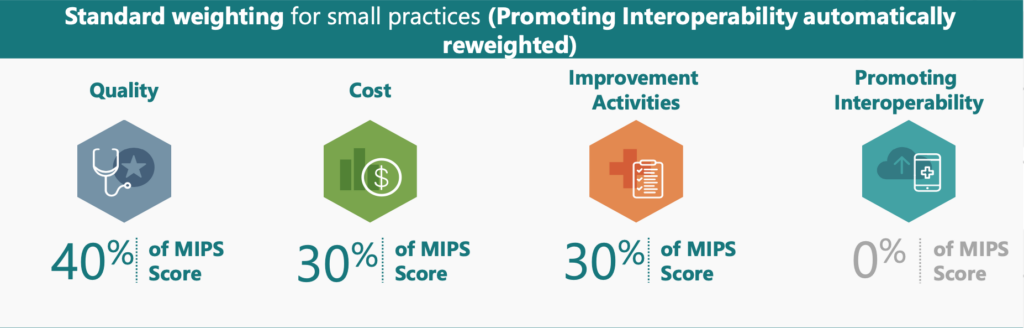
The most significant difference in MIPS reporting between small and large practices is that small practices qualify for Automatic Reweighting of the Promoting Interoperability (PI) Performance Category. This means that small practices are not required to submit any PI data. Instead, the Quality Performance Category will be reweighted to represent 40% of your overall final score, and Improvement Activities will represent 30% (see table below)
Improvement Activities are double weighted for small practices. This means that medium weighted activities are worth 20 points, and high weighted activities are worth 40 points (compared to 10 points and 20 points respectively for large practices).
Another difference is that only small practices are permitted to submit Medicare Part B claims measures in the Quality performance category. Small practices will also receive 3 points for a quality measure that doesn’t reach 70% data completeness, versus 0 points for large practices. Also, 6 bonus points are automatically added to the Quality category if data for at least 1 quality measure is reported.
You can read more about these similarities and differences from the College of American Pathologists, as well as from the official CMS website.
