In August 2023 CMS released performance feedback, final scores, and payment adjustments for clinicians who participated in PY22 MIPS. The result of these scores will directly affect Medicare reimbursements for covered professional services beginning Jan 1, 2024. Luckily, if you believe that CMS made a mistake when calculating your score or payment adjustment, you can request a Targeted Review, and CMS will review your submission for any errors. The deadline to request a Targeted Review is October 9, 2023.
Who can Submit a Targeted Review?
You are eligible to submit a targeted review if you are:
- MIPS eligible clinician
- Group
- Virtual Group
- APM Participant
What can/can’t I Request a Targeted Review For?
You can request a targeted review if you find an error with your 2022 MIPS performance feedback and associated 2024 MIPS payment adjustment factor(s). The following circumstances would qualify for a targeted review request:
- Your performance data was submitted under the incorrect Taxpayer Identification Number (TIN) or National Provider Identifier (NPI).
- You qualified for performance category reweighting because of a special status designation, Promoting Interoperability Hardship Exception, or Extreme and Uncontrollable Circumstances Exception that was incorrectly applied.
However, there are certain elements of your submission that will NOT permit a targeted review, such as the following:
- The methodology used to establish the amount of the MIPS payment adjustment factor, the amount of the additional MIPS payment adjustment factor, and the determination of such amounts.
- The identification of measures and activities specified for a MIPS performance category and information made public or posted on Medicare Care Compare.
- The developed methodology used to calculate performance scores and the calculation of such scores, including the weighting of measures and activities under such methodology.
Keep in mind that these aren’t comprehensive lists of circumstances. If you have questions about whether your circumstances warrant a targeted review, you can contact the Quality Payment Program by email at QPP@cms.hhs.gov.
How to Submit a Targeted Review
The following timeline shares a brief, step-by-step layout of how to submit a targeted review:
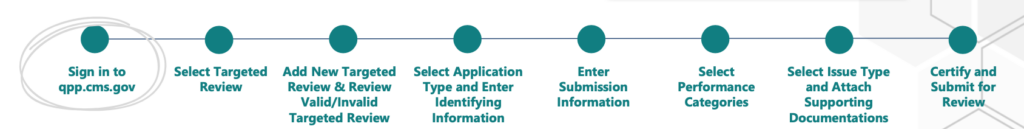
Step 1: Sign into your QPP account using HARP credentials on the QPP website.
- Don’t have a HARP account? You can register for one here.
Step 2: Select ‘Targeted Review’ from the left-hand navigation pane.
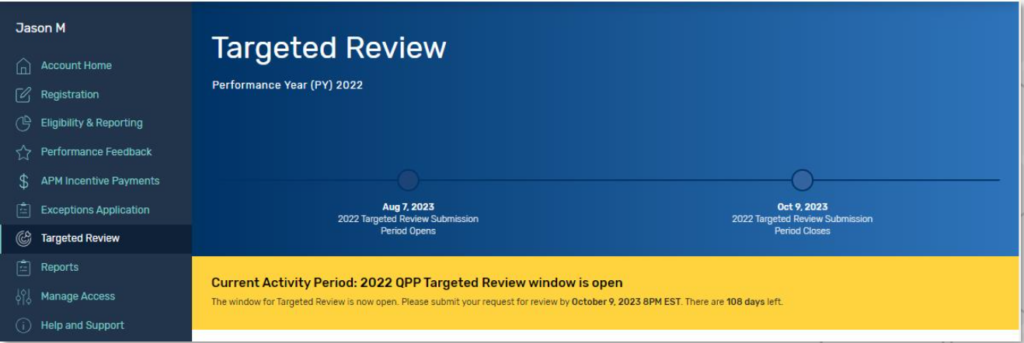
Step 3: Select ‘Add New Targeted Review’ to create an application.
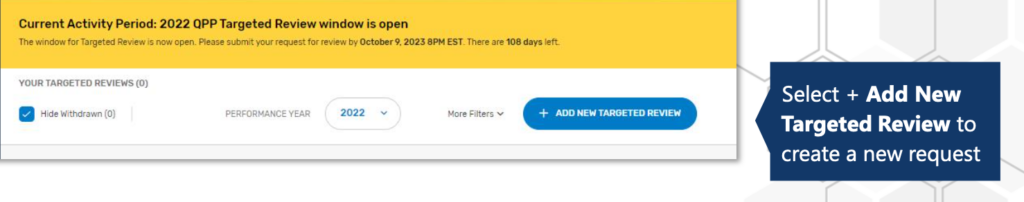
You should then review the valid and invalid targeted review examples provided to you.
Step 4:
- Select the application type that aligns with how your data was submitted to MIPS for the 2022 calendar year. Then select Save & Continue.
- Enter the required identifying information based on which application type you choose. Each application type requires a different type of identifying information (for example, individual – NPI; group – TIN).
Step 5: Submit your information
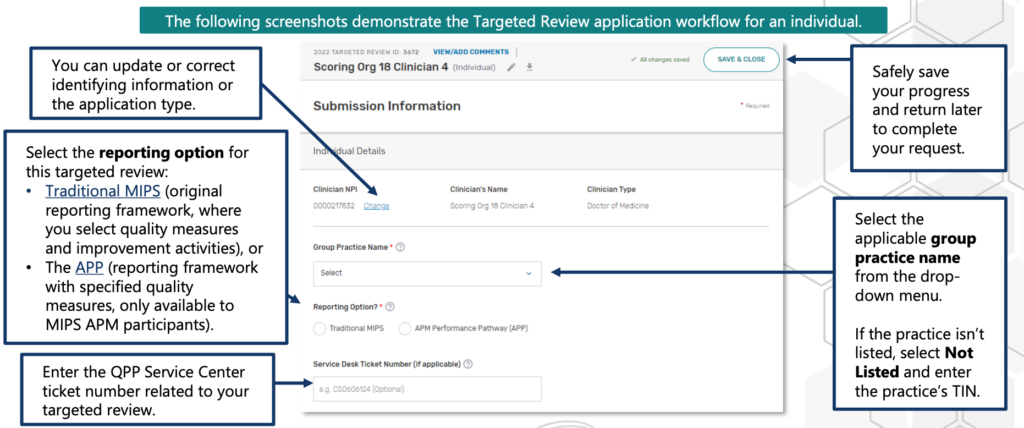
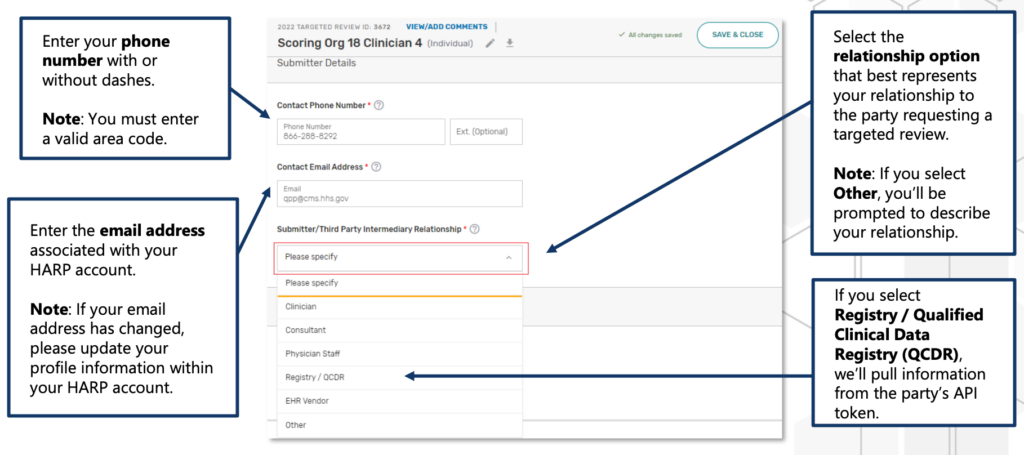
You can provide additional staff or representatives’ email addresses for notification purposes regarding the request status. If you enter an email associated with an individual’s HARP account, they will access the Targeted Review application and receive notifications upon signing in with their HARP credentials on the Quality Payment Program website. For applications on behalf of individuals, groups, or virtual groups, those with access to the respective practice or virtual group on the Quality Payment Program website can only access the application if their HARP-associated email is added.
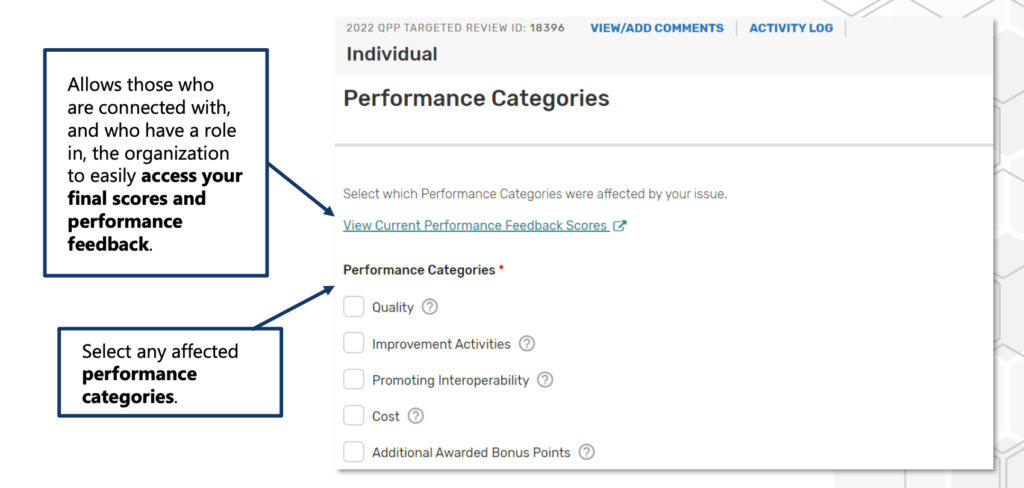
Step 6: Select the performance categories that were affected by the issue(s) you experienced.
Step 7:
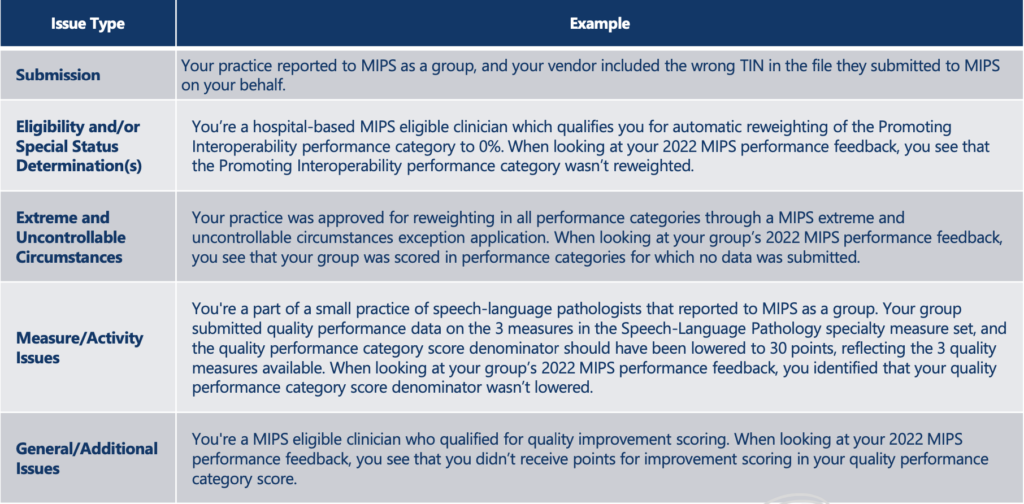
a) Select the applicable issue type(s) that best describe the issue(s) you identified with your 2024 payment adjustment factor(s) and associated 2022 final performance feedback. Then provide a detailed explanation of the issue(s) you identified. The following shows examples of issue types:
b) Attach your supporting documents, which may include:
- Extracts from the MIPS eligible clinician’s EHR.
- Copies of performance data provided to a third-party intermediary by the clinician or group.
- Copies of performance data submitted to CMS
Step 8: Read the disclosure, then press Certify & Submit
Following these steps, you’ll be brought back to the Targeted Review Progress Summary page. You’ll see a pop- up message confirming that you successfully submitted your review. You will also receive an email confirming your application.
You’ll be able to monitor the progress of your request on the Targeted Review Progress Summary page. Select View Details for additional information about a specific request.
You can also communicate with your reviewer by selecting View Details and use the Comments function to communicate with the reviewer and submit supporting documentation for your request.
CMS may require documentation to support a targeted review request, which varies by circumstance. A CMS representative will contact you about providing any specific documentation if required. If the targeted review request is approved and results in a scoring change, CMS will update your final score and/or associated payment adjustment (if applicable). Please note that targeted review decisions are final and not eligible for further review.
The deadline for submitting a Targeted Review is October 9, 2023, and if you need any more assistance, you can contact one of our MIPS experts by logging in or signing up at our MIPS portal.
