With the release of the 2024 Quality Payment Program (QPP) Final Rule, clinicians, groups, and participants have many questions related to new program features and changes. Here are some of the most frequently asked questions according to CMS:
How do I know if I’m eligible for MIPS in 2024?
Answer: According to CMS, to be eligible for MIPS, you must:
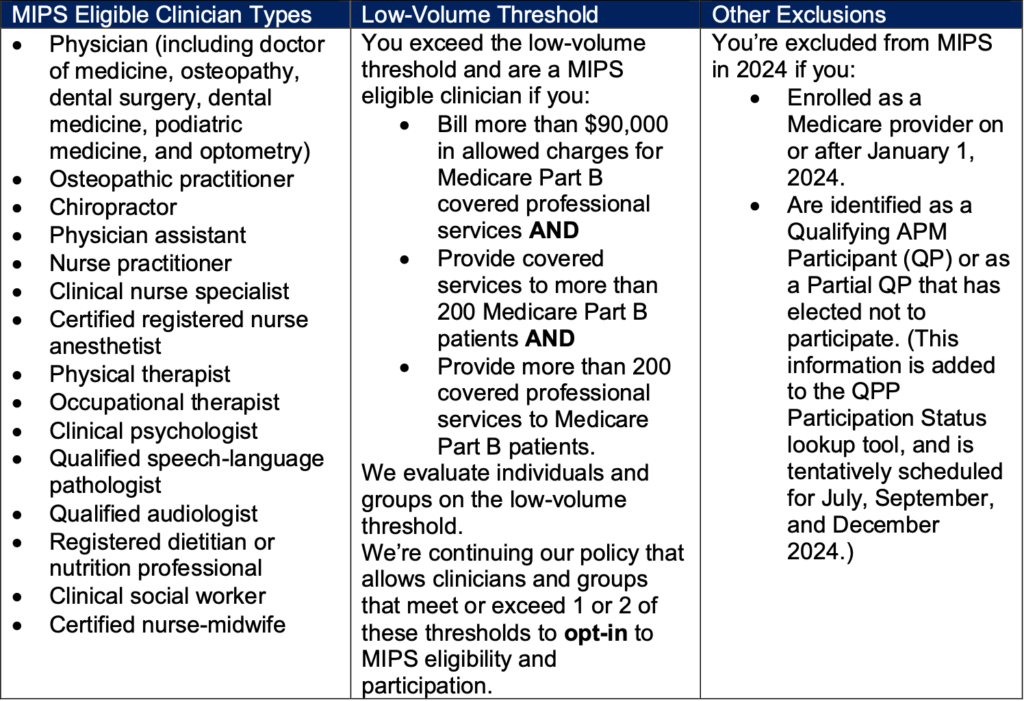
- Be a MIPS eligible clinician (see the chart below)
- Exceed the low-volume threshold as an individual or group
- Not be otherwise excluded because of your Medicare enrollment date or your status as a Qualifying APM Participant (QP), or as a Partial QP that has elected not to participate
Are there any changes to reporting requirements?
Answer: Two of the most significant changes are to the Promoting Interoperability and Quality performance categories. For the Promoting Interoperability category, CMS has increased the length of the performance period to a minimum of 180 continuous days. For the Quality performance category, the data completeness threshold for reporting quality measures has been increased to 75%.
Can clinicians still use a third-party health IT vendor to assist in data collection and submission?
Answer: Yes! However, beginning next year in the 2025 performance year, third party vendors will not be allowed to assist with submission UNLESS they are a Qualified Clinical Data Registry (QCDR) or Qualified Registry. HCIS is a CMS Qualified Registry, meaning we can assist in your data collection and submission for this year AND next.
If my practice is transitioning to a new EHR system mid-year, how will it affect my Quality reporting?
Answer: CMS wants to emphasize that the 12-month performance period and 75% data completeness threshold are applicable regardless of any EHR system transition. This means that you, the clinician or group, will have to report data with BOTH EHR systems, meaning you’ll have to collect data before and after your transition, and aggregate the data into a single 12-month report for submission.
When will measure specifications and supporting documentation be available for finalized measures?
Answer: Measure specifications and supporting documentation is available now at the QPP Resource Library. Scroll past the General and Regulatory sections until you find ‘Full Resource Library’, where you can filter for PY24.
What new MIPS Value Pathways (MVPs) are available for reporting in 2024?
Answer: There are five new MVPs available for 2024.
- Focusing on Women’s Health
- Quality Care for the Treatment of Ear, Nose, and Throat Disorders
- Prevention and Treatment of Infectious Disorders Including Hepatitis C and HIV
- Quality Care in Mental Health and Substance Use Disorders
- Rehabilitative Support for Musculoskeletal Care
We’ll dive more into these new MVPs in a future blog.
Resources
- 2024 Quality Payment Program Final Rule
- 2024 QPP Final Rule MVP Guide (PDF)
- Transition from Traditional MIPS to MVPs (PDF)
And be sure to check out our previous blogs at www.healthcareinnovationsolutions.com/blog.
