Since the inception of the Merit-Based Incentive Payment System (MIPS), the Centers for Medicare & Medicaid Services (CMS) has provided special designations and rulings for clinicians reporting as “small practices”. According to CMS, a small practice is defined as “a group that has 15 or fewer clinicians identified by National Provider Identifier (NPI), billing under the group’s Taxpayer Identification Number (TIN).” The following information will be helpful to small practices looking to report and submit data for 2024 MIPS.
Quality Performance Category
There are some differences in reporting between small and regular practices when it comes to the Quality category:
- Small Practices will automatically receive 3 points for submitting:
- Quality measures without an available benchmark (historical or performance period).
- Quality measures that don’t meet the case minimum (20 eligible denominator cases).
- Quality measures that don’t meet data completeness requirements (75% for PY24).
- Small practices who submit at least 1 quality measure will continue to earn 6 bonus points. (This bonus isn’t added to clinicians or groups who are scored under facility-based scoring.)
- Note: CMS will only calculate a group-level quality score from Medicare Part B claims measures if the practice submits group-level data in another performance category.
Improvement Activities Performance Category
This category will have the same adjustments in requirements for small and rural practices as they did in 2023. Small practices continue to receive double weighting for each activity. These types of practices will receive full credit if they perform and attest to the following:
- 1 high-weighted activity OR 2 medium-weighted activities for traditional MIPS or MVP (all eligible clinicians reporting an MVP receive this flexibility not just small practices).
- All clinicians automatically receive full credit in this performance category in the 2024 performance year when reporting the APP.
If a small practice is reporting as a group at least 50% of the clinicians in the group must perform the same activity for a continuous 90-day period to attest and receive credit for that activity.
Promoting Interoperability Performance Category
For small practices, this category will be automatically reweighted to represent 0% of your final score. Small practices are not required to report or submit data in this category, and submitting a hardship exception is not necessary to reweight this category. However, if they submit any Promoting Interoperability data the performance category will be scored and will represent 25% of your final score.
Performance Category and Final Score Redistribution
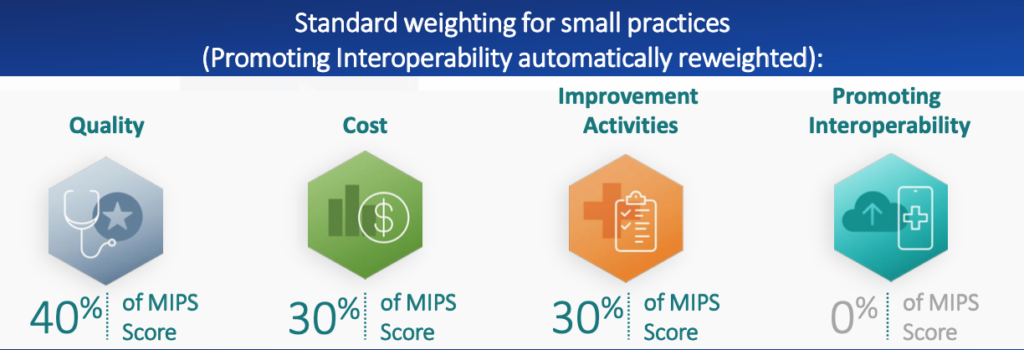
The normal circumstance for small practices, in which only the Promoting Interoperability category is reweighted, would result in this final score distribution:
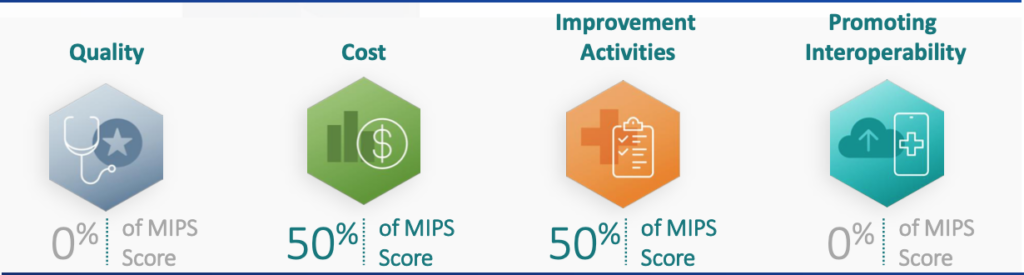
When both the Promoting Interoperability and Cost categories are reweighted, the resulting distribution will be as follows:

In a case where the quality category is reweighted, along with the Promoting Interoperability category, the distribution would appear as so:
Resources:
- Healthcare Innovation Solutions (HCIS) Blog – Find more information on MIPS for Performance Years (PY) 23 and 24
- CMS page on Small Practices
- CMS Small Practice Guide for MIPS PY24
