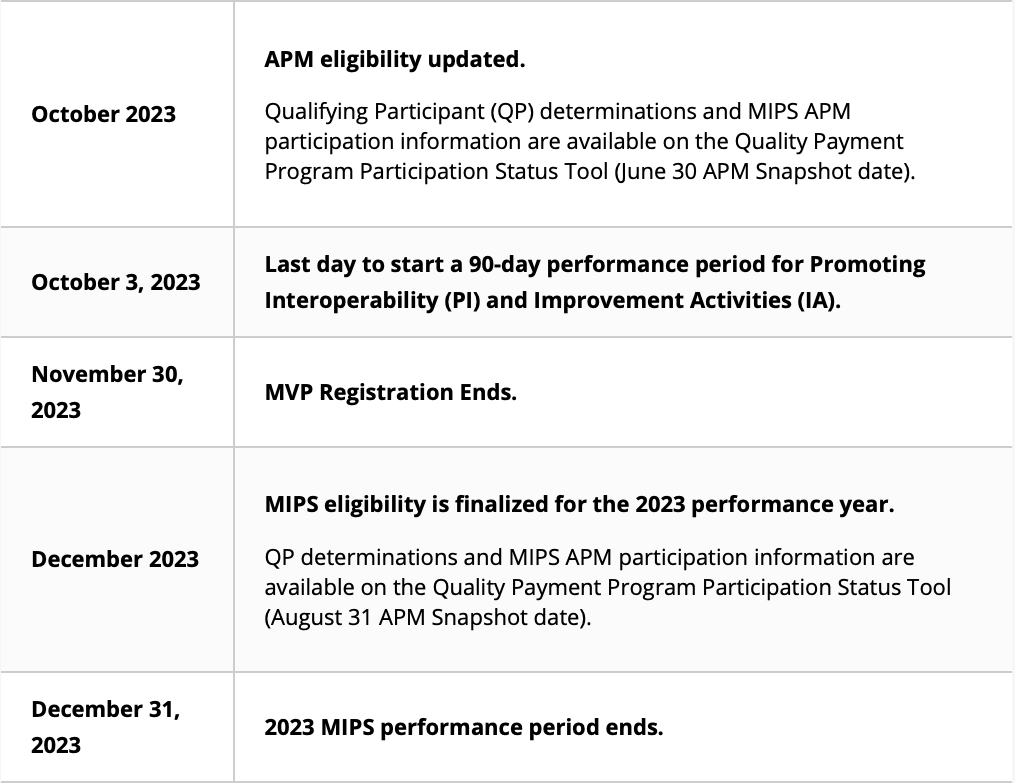
Ready or not, Quarter 4 of the 2023 MIPS Performance Year is almost here, and HCIS wants to assist all eligible clinicians and groups throughout the data collection and submission processes. The timeline for the rest of the performance year is as follows:
Depending on where you are in the process, the period between now and December could play a large role in terms of capturing your data, submissions, and Final Score. The following 7 tips are designed to help you optimize your performance in each category, recognize any need you may have for a reweighting or exception, and ensure the smoothest possible Quarter 4 for PY23.
Tips for a Successful PY 2023 Submission
Tip #1 – Choose Your Quality Measures Wisely
- Select at least 6 Quality Measures (or specialty measure set)
- Choose measures that are already being tracked in your EHR to minimize workflow changes and avoid manual data collection
- If you are not using an EHR to collect data for the measures, you can use CMS Specialty Measure Sets and select measures that are specific to your practice and documented often
Tip #2 – Follow the Reliable Scoring Criteria for Quality Measures
- In order to score the max points for a measure a clinician/group must:
- Meet the 70% reporting threshold (reflects ALL payers, not limited to Medicare Part B)
- Clinicians are required to have at least 20 denominator eligible cases for each measure
- Measure should have a benchmark
- If a measure reported does not meet the criteria above the clinician/group will earn the minimum amount of points
- 3 points for small practices, and 0 points for large practices
Tip #3 – Report the Required Promoting Interoperability Measures or Claim the Exclusions if Applicable
- Complete Security Risk Analysis and SAFER Guide by 12/31/2023
- Report the following required objectives (or claim the applicable exclusions)
- E-prescribing.
- Health Information Exchange.
- Provider to Patient Exchange.
- Public Health and Clinical Data Registry Reporting.
Tip #4 – Don’t Forget about your Patient Portal
- Provide patient electronic access to their health information.
- 25% of your overall Promoting Interoperability score
- If exclusions are taken this measure can be up to 90% of your PI score.
- Ways to improve:
- Check with your EHR vendor on ways to make it easier for your patients to access their portal.
- Make sure your portal is activated!
- Incorporate the patient portal into the workflow of your patient’s visit.
- Spread awareness through your office to encourage use of the portal with patients.
Tip #5 – Practices can apply for the Promoting Interoperability Hardship Exception or may Qualify for Automatic Reweighting
- Small practices qualify for automatic reweighting of the Promoting Interoperability performance category
- The 25% category weighting will be redistributed to another performance category or categories
- Will not need to submit a Promoting Interoperability hardship exception application
- Submitting data cancels reweighting
- Promoting Interoperability performance will count for 25% of your MIPS final score.
- You may submit a MIPS Promoting Interoperability hardship exception application (by 1/2/2024) if any of the following reasons apply.
- You’re using decertified EHR technology.
- You have insufficient internet connectivity.
- You experience an extreme and uncontrollable circumstance.
- You lack control over the availability of the CEHRT.
- You can learn more about MIPS Exception Applications from our previous blog.
Tip #6 – Make sure you Earn the Maximum Number of Points for the Improvement Activity Performance Category
- To earn full credit for the improvement activities category, small practices should report on the following:
- 1 high-weighted activity OR
- 2 medium-weighted activities.
- To earn full credit for the improvement activities category, large practices should report on the following:
- 2 high-weighted activities OR
- 1 high-weighted activity & 2 medium-weighted activities OR
- 4 medium-weighted activities.
- Recommended Improvement Activities
- Provide 24/7 Access to MIPS Eligible Clinicians or Groups who have Real-Time Access to Patient’s Medical Record (applicable for cloud-based EHRs).
- Use of telehealth services that expand practice access.
Tip #7 – Register in Advance to Report an MVP
- For the 2023 performance year, you can choose to report an MVP in addition to another reporting option, such as traditional MIPS or the APP, and CMS will take the highest score you receive.
- Select 4 Quality measures from the set of MVP specific measures.
- This includes one outcome measure or high priority measure in the absence of an available outcome measure.
- This can include an outcomes-based administrative claims measures (automatically calculated if selected during MVP registration).
- Report performance data for at least 70% of the denominator eligible cases for each quality measure.
- Must have at least 20 denominator eligible cases for each measure.
- You can submit measures from different collection types to meet quality performance category reporting requirements.
- eCQMs, MIPS CQMs, and QCDR measures include all-payer data.
- Only Medicare Part B claims measures are limited to Medicare patients/encounters.
Please be on the lookout for more blog posts in the coming weeks and months, as this is a crucial time for all MIPS eligible clinicians.
