On August 12th, the Centers for Medicare & Medicaid Services (CMS) delivered Final Score previews and performance feedback for the Merit-Based Incentive Payment System (MIPS) Performance Year 2023 (PY23). All clinicians who participated in MIPS PY23 can view their Final Score preview via the Quality Payment Program (QPP) website. These results will determine your payment adjustment in 2025, making it crucial to review this information carefully. Any errors in CMS’s calculation of your data could negatively affect your payment adjustment. If errors are found, you may be eligible for a targeted review, ensuring that you receive the correct payment adjustment.
Targeted reviews for PY23 must be submitted by October 11th, 2024, at 8 PM EST.
Why Request a Targeted Review?
Requesting a targeted review helps ensure that any errors in your MIPS feedback are corrected, potentially saving you from a lower payment adjustment. A successful review can protect your practice from unnecessary financial penalties and ensure your performance is accurately represented.
Who Can Request a Targeted Review?
Any clinician type that is MIPS-eligible and participated in PY23 can request a targeted review. This includes individual clinicians, groups, virtual groups, and subgroups, whether you reported under Traditional MIPS or using a MIPS Value Pathway (MVP).
What Errors Qualify for a Targeted Review?
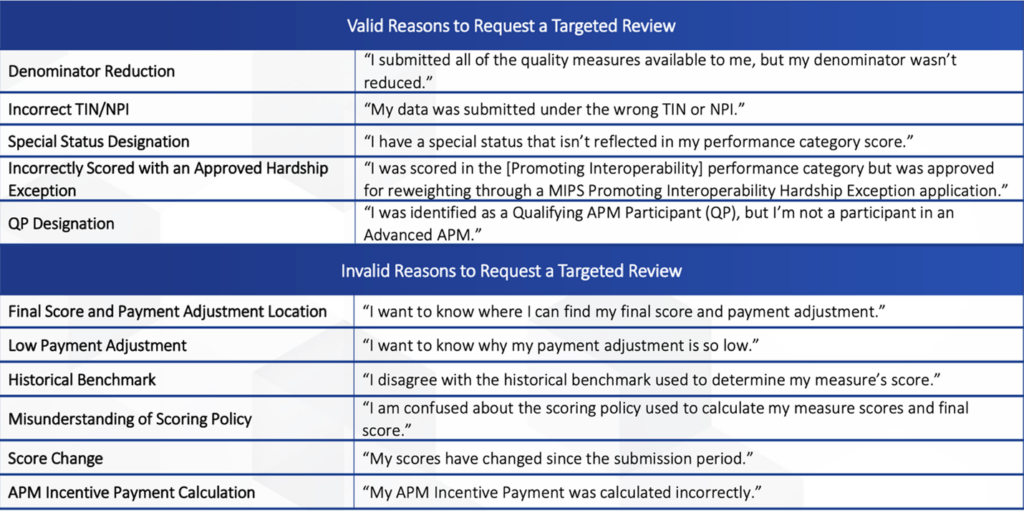
Targeted reviews focus on correcting errors in the payment adjustment calculations based on Final Scores. According to CMS, the following scenarios qualify for a targeted review:
- Your performance data was submitted under the incorrect Taxpayer Identification Number (TIN) or National Provider Identifier (NPI).
- You qualified for performance category reweighting because of a special status designation, Promoting Interoperability Hardship Exception, or Extreme and Uncontrollable Circumstances Exception that was incorrectly applied.
However, a targeted review WILL NOT be performed for disputes regarding:
- The methodology used to calculate performance scores or the weighting of measures.
- The methodology for determining the amount of the MIPS payment adjustment factor.
This graphic provides more examples of what qualifies for a targeted review:
How Should I Prepare for a Targeted Review?
Before submitting a targeted review, CMS recommends gathering all relevant documentation related to your request. These documents may include:
- Extracts from your Electronic Health Record (EHR)
- Copies of performance data submitted to CMS or third-party intermediaries
- QPP Service Center case numbers
Attaching supporting documentation to your initial request can streamline the review process.
Need Assistance?
Healthcare Innovation Solutions (HCIS) is your partner for all things MIPS. If you’d like to speak with one of our advisors, you can schedule a FREE 15-minute consultation by clicking here.
