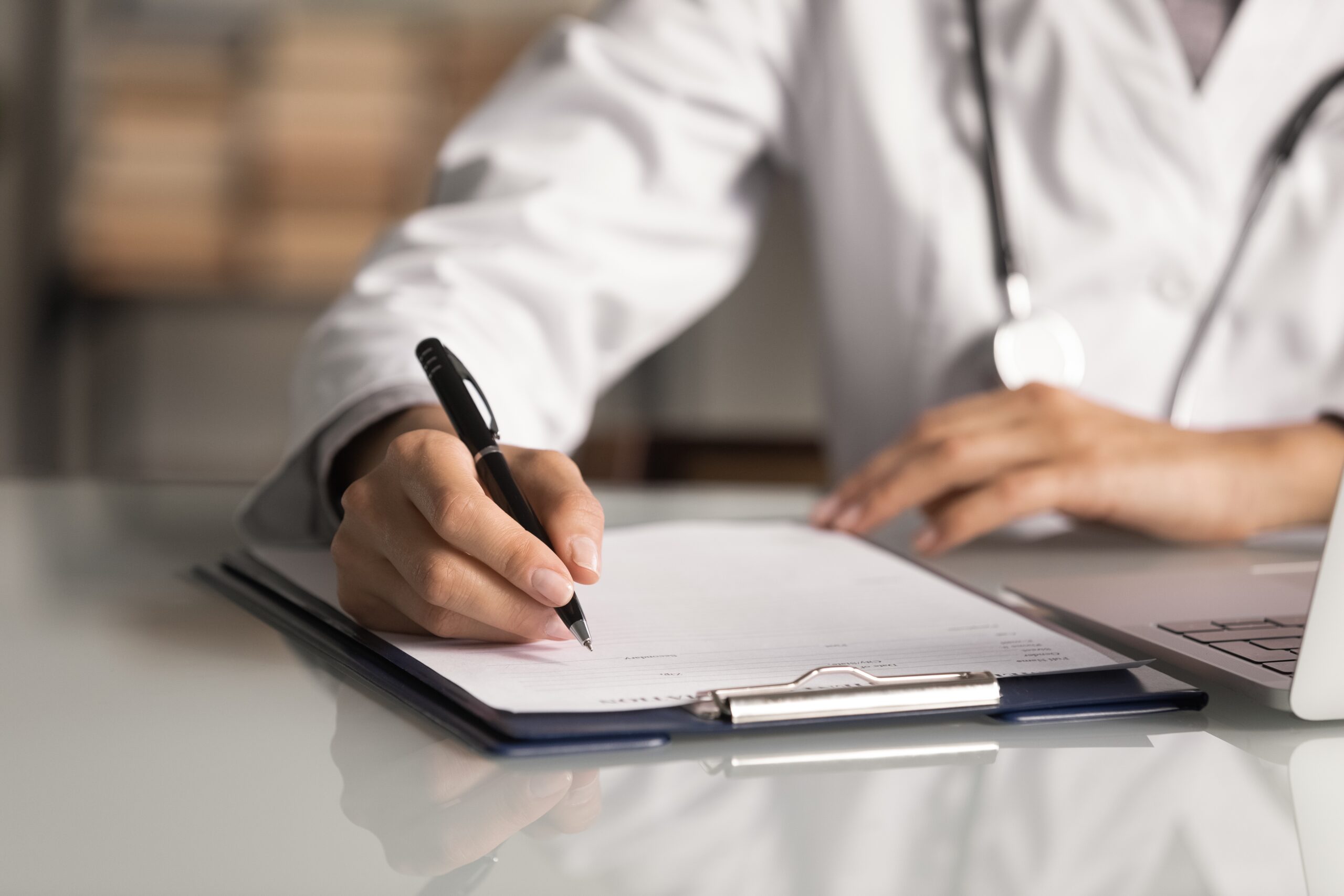
MIPS Program Overview
The Merit-Based Incentive Payment System (MIPS) is a flagship reimbursement program from the Centers for Medicare and Medicaid Services (CMS) under the Quality Payment Program (QPP). By assessing an eligible clinician’s performance within four categories (Quality, Cost, Improvement Activities, and Promoting Interoperability), MIPS weighs and transforms your data into a final score (between 1 and 100), which is weighted against a benchmark (75 points in Performance Year 24 (PY24)). Depending on a clinician’s final score, they will receive either a positive or negative payment adjustment for the payment year, which is two years following the submission year.
We help eligible providers avoid penalties and maximize their potential earnings by optimizing their scores and meeting all their reporting requirements. For 2024, eligible providers can be subjected to a -9% penalty on their 2026 Medicare Part B payments or earn up to 9% in financial incentives.
For more information regarding the Merit-Based Incentive Payment System (MIPS) visit the Quality Payment Program website by clicking here.
Software
The MIPS Submission process requires use of a CMS Certified Registry. The MIPS Portal is our user friendly, proprietary submission software. MIPS Portal allows eligible clinicians to easily view, organize, customize, and save the preferences and measures of their submission. Get started today!
Who Is Eligible for the MIPS/MVPs Program?
MIPS/MVPs participation is mandatory for many clinicians that meet these criteria:
- Have more than 200 Medicare Part B patients,
- Have more than $90,000 in associated medical billing per year, and
- Cover more than 200 Medicare professional services during the performance period.
Participants also need to be one of the following types of clinicians:
- Physicians
- Physician Assistants
- Nurse Practitioners
- Clinical Nurse Specialists
- Certified Registered Nurse Anesthetists
- Clinical Psychologists
- Physical Therapists
- Occupational Therapists
- Speech/Language Pathologists
- Audiologists
- Nutrition Professionals
Visit our FAQ page for more!
Performance Year Timeline
- 2024 Performance Year:
- January 1 to December 31 Clinicians care for patients and record data during the year.
- 2025 Data Submission:
- Deadline for submitting data is in Spring 2025 Clinicians are encouraged to submit data early.
- 2025 Feedback:
- CMS provides performance feedback after data is submitted. Clinicians will receive feedback before the payment year starts.
- 2026 Payment Adjustment:
- MIPS payment adjustments are prospectively applied to each claim beginning January 1.

Program Highlights
4,300+
client practices submitted

$12M
incentives earned
$47M
penalties avoided
Introduction to MIPS Value Pathways (MVPs) for 2024
MVPs are a reporting option that offers clinicians a subset of measures and activities relevant to a specialty or specific medical condition. Clinicians can select, collect, and report on a reduced number of quality measures and improvement activities as compared to traditional MIPS. However, you are still required to report on the complete Promoting Interoperability (PI) measure set. CMS will collect and calculate data in the Cost Performance category and Population Health Measures.
Schedule a FREE 15-minute consultation!
Choose a time that works for you and our advisors will you have questions about MIPS reporting requirements or want to better understand your eligibility or reporting requirements, please make an appointment with our MIPS advisors.
How Can I Participate?
You can register now to submit through our CMS qualified registry or engage with our MIPS advisors for support. For more detail on our services and pricing click here. Contact us below if you have additional questions.
